Expert proctology support to ensure safe, effective, and lasting recovery.
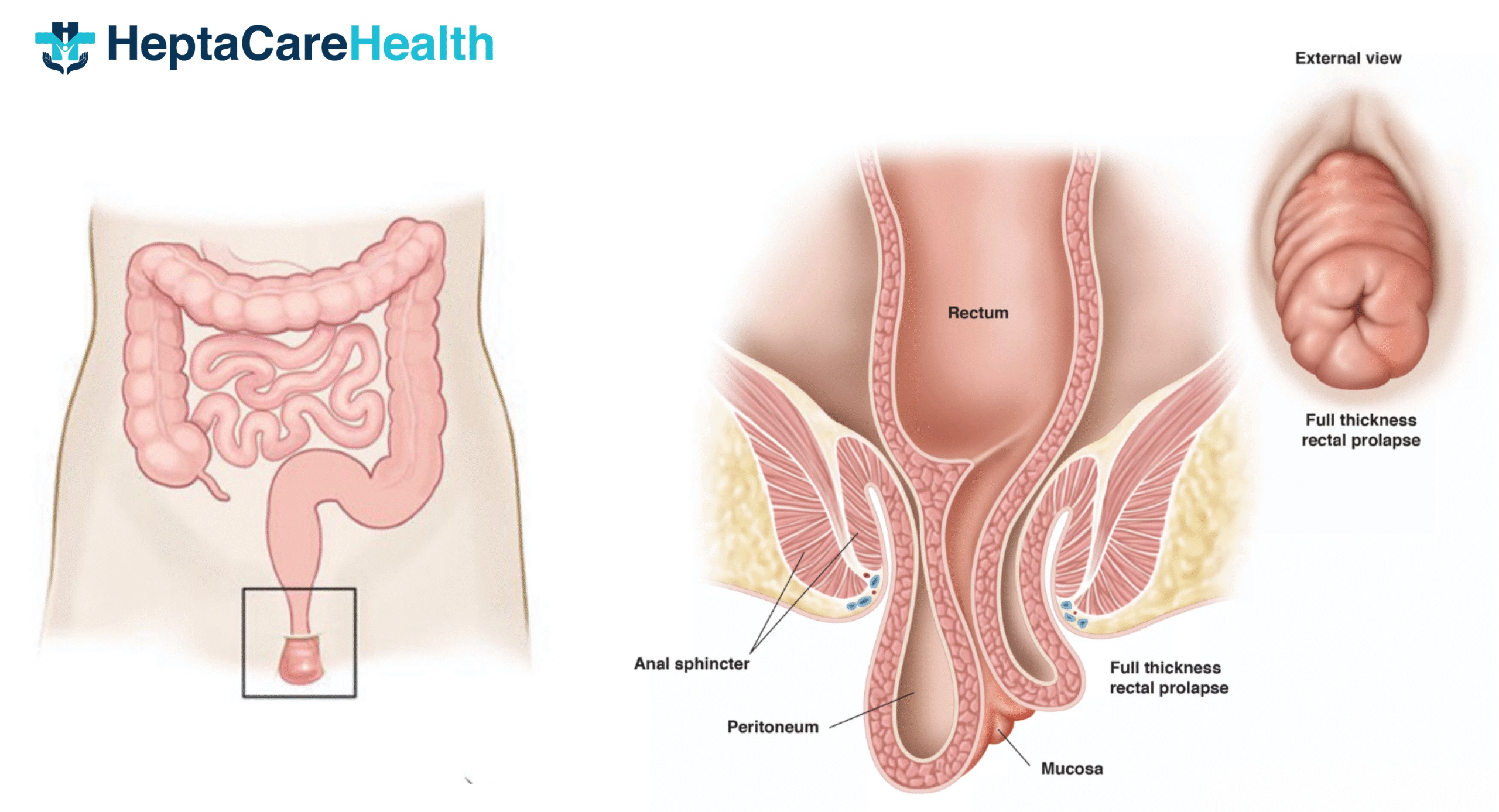
Rectal prolapse is a proctological condition in which the rectum slides down the anus and often leads to potential complications such as strangulation of the rectum, bleeding, and ulceration. Therefore, timely treatment is a must. At HeptaCare Health, we provide advanced surgical treatments for Rectal Prolapse and help patients get relief from the discomfort caused by this condition. Book your appointment with our proctologists now!
Happy Patients
Disease
Hospitals
Cities
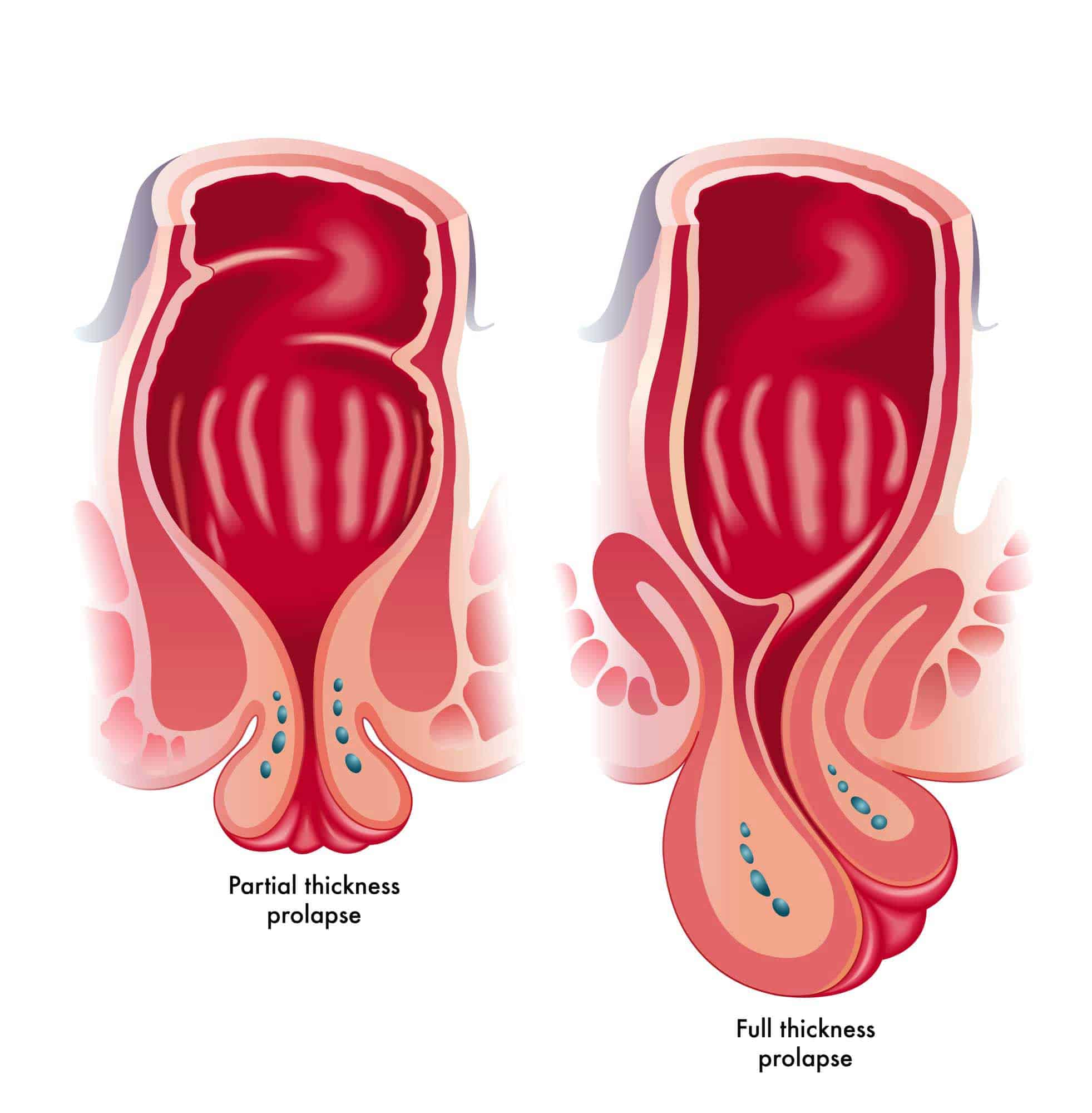
The rectum is located at the end of the large intestine. It is the section of the digestive tract where the stool is held before it passes through the system. When the stool reaches the rectum, you may experience an urge to defecate. A group of muscles push the stool out of the anus. A rectal prolapse occurs when the rectum is pushed out along with the stool. The word ‘prolapse’ is used when any organ of the body slips from its original position.
Rectal prolapse is more common in women than in men and generally affects people over 50 years or those who have a history of chronic constipation or diarrhoea.
Rectal Prolapse Diagnosis
The complete diagnostic procedure for rectal prolapse includes:
Physical Examination: In the physical examination, the doctor observes the rectum and may insert a gloved and lubricated finger in the anus to check the strength of the anal sphincter and the rectum. In this exam, the doctor will ask you to describe your symptoms and medical history to understand the condition better. They may even ask you to squat and strain as you do during the bowel movement.
Based on the findings of the physical assessment, the doctor might ask you to get some other tests done.
Anal electromyography (EMG): This test lets doctors measure the effectiveness of muscles and nerves in the rectum. The doctors place electrodes a few inches into the rectum to perform this test. The procedure takes a few minutes.
Colonoscopy: This diagnostic procedure involves the insertion of a thin and flexible tube with a small camera (colonoscope) into the rectum to perform a visual exam of the area.
Anorectal manometry: In this test, doctors use a flexible tube which is the size of a thermometer and has a small deflated balloon attached to its end to measure the rectum’s response to pressure. The device is inserted into the rectum before conducting the test.
Barium enema: In the Barium Enema test, the doctors place a chalky liquid containing barium in the rectum of the patient. The barium becomes visible on the X-rays, producing clear images of the area.
Defecography: In this test, the doctors use x-rays or MRIs to monitor your colon as you have a bowel movement.
Lower GI series: To perform this test, doctors place a chalky liquid containing barium in the large intestine of the patient. This liquid lets doctors get a clear picture of the area on an X-ray.
Transit study: In this test, the doctor asks the patient to swallow one or more capsules which have markers on them. These markers can be seen on the X-ray. After swallowing the capsules, the patient has to appear for x-rays for the next 5 days. It helps doctors assess how the markers pass through the intestines.
In some cases, the doctor might suggest urological
or gynaecological exams to check for weak areas in the pelvic floor and see if other organs, such as the uterus, have prolapsed as well.
There are various surgical treatment options for rectal prolapse, including;
Rectopexy, also called rectal prolapse surgery, involves repairing the rectum through the abdomen. Surgeons typically perform the procedure under general anesthesia, and patients usually stay in the hospital for several days. Recovery time varies, but most people return to normal activities within a few weeks. Doctors consider rectopexy a safe and effective treatment for rectal prolapse, with a high success rate in preventing the condition from recurring. Here’s how the surgery works:
1. During a rectopexy procedure, the surgeon will make an incision in the abdomen.
2. The surgeon will then locate the rectum and dissect it carefully from the surrounding tissues.
3. After this, the surgeon will suture the rectum to the sacrum and will ensure that the rectum is properly positioned.
4.The surgeon will then close the incision in the abdomen with sutures or staples.
5.The patient will be monitored closely following the procedure to ensure proper healing.
Laparoscopic rectal prolapse surgery is a minimally invasive procedure that is used to treat rectal prolapse. This surgery is performed through small incisions in the abdomen rather than a large incision in the rectum. This approach has many benefits, including less pain, faster recovery times, and a lower risk of complications. Patients who undergo laparoscopic rectal prolapse surgery can typically return to their normal activities within a few weeks. Here’s an explanation of the steps involved in a laparoscopic rectal prolapse surgery to help you understand the procedure properly:
1: The surgeon will administer general anesthesia to the patient.
2: After the patient is sedated, the surgeon will insert a laparoscope into the abdomen.
3: The surgeon will make small incisions in the abdomen to insert surgical instruments.
4: The surgeon will locate the rectum and gently pull it out of the body.
5: The surgeon will remove any excess tissue or prolapsed areas from the rectum.
6: The surgeon will suture the rectum back into place.
7: The surgeon will close the incisions with sutures or staples.
8: The patient will be monitored in the recovery room before hospital discharge.
Robotic surgery for rectal prolapse is a minimally invasive surgical procedure that offers several benefits over traditional open surgery. These benefits include reduced blood loss, less pain and scarring, and shorter hospital stays. Recovery time after robotic surgery for rectal prolapse is typically shorter than with open surgery, with most patients able to return to normal activities within a few weeks. Here’s how a robotic surgery for rectal prolapse is performed:
Perineal Rectosigmoidectomy is a surgical procedure that removes part of the rectum and sigmoid colon via the perineum. Benefits include faster recovery time and lower risk of complications. Recovery time varies but is generally shorter than traditional surgery. This surgery is performed in the following steps:
The Delorme procedure is another surgical treatment for rectal prolapse. It involves folding and sewing a portion of the rectal wall to itself to reinforce weak or damaged tissue. Benefits include improved bowel function and reduced risk of recurrence. Recovery time varies but typically takes 2-4 weeks. The steps of the Delorme procedure for rectal prolapse treatment are as follows:
Laser rectal prolapse surgery offers various benefits, including;
Overall, laser rectal prolapse surgery is a safe and effective option for patients seeking relief from the symptoms of rectal prolapse.
If your doctor suggested rectal prolapse surgery, then it is important for you to be prepared for the procedure. Here are some suggestions that you can follow to prepare for your rectal prolapse surgery.
It may take you up to 4–6 weeks to recover completely after the surgery. Here are general guidelines to help you recover faster after laser rectal prolapse surgery:
After rectal prolapse surgery, it is important to take medicines on time as prescribed by your doctor.
You may experience discomfort and swelling in the surgical area, which can be managed with ice packs and medicines.
Avoid lifting heavy objects or engaging in strenuous activities for several weeks after surgery.
Eat a high-fiber diet to avoid constipation and straining during bowel movements.
Drinking plenty of water and staying hydrated can also help prevent constipation.
Your doctor may recommend stool softeners or laxatives to help ease bowel movements.
Follow any post-surgery care instructions given by your doctor or healthcare team.
You may experience some bleeding or discharge after surgery. This is normal and should subside within a few days.
It is important to attend all post-surgery follow-up appointments to monitor your recovery progress.
If you experience severe pain, fever, or other concerning symptoms, contact your doctor immediately.
After undergoing rectal prolapse treatment through surgery, some lifestyle changes need to be made in order to ensure proper healing and prevent future occurrences. These changes include:
Individuals who have undergone rectal prolapse treatment through surgery can improve their overall health and reduce the risk of recurrence by making these lifestyle changes. It is important to follow these guidelines as recommended by a healthcare professional.
While rectal prolapse surgery is an effective option but it comes with some risks and complications, including;
Rectal prolapse treatment without surgery can relieve symptoms such as pain and discomfort at its initial stage, but it is not the best option to treat the condition.
Here are some non-surgical options to relieve symptoms or prevent the condition.
If you are experiencing rectal prolapse, there are several home remedies you can try to prevent rectal prolapse
It is important to note that while these home remedies may provide relief, they are not a substitute for medical treatment. If you are experiencing rectal prolapse, it is important to consult with an experienced proctologist to determine the underlying cause and appropriate treatment options.
Here are some signs that indicate that your rectal prolapse is healing.
Untreated rectal prolapse can lead to various severe complications, including;
If you’re diagnosed with a rectal prolapse, it is important that you make somyou must makee changes to your diet. Listed below are some foods you should avoid if you have a rectal prolapse:


Based on 7721 Recommendations | Rated 4.68 Out of 5
Happy Patients
Clinics
Cities
Surgeries
Doctors
Hospitals
Advanced, non-surgical care for painful anal fissures with quick relief and minimal downtime.
Expert proctology support to ensure safe, effective, and lasting recovery.

Get relief from painful piles with advanced laser treatment.
Minimally invasive, no stitches, same-day discharge…
Heal painful anal fissures with advanced, non-surgical care.
Quick relief, minimal downtime, expert proctology support…

Get permanent relief from pilonidal sinus with laser surgery.
Painless procedure, quick healing, same-day discharge.

Advanced treatment for fissure by expert surgeons.
Safe procedure, minimal pain, long-term relief.

Common symptoms include itching, pain during bowel movements, bleeding, and swelling around the anus.
Yes, most health insurance plans cover rectal surgery, including laser treatment.
Eat a high-fiber diet, drink water, avoid straining during bowel movements, and exercise regularly.
It’s a safe and effective method with minimal side effects and faster healing than traditional surgery.
● piles laser surgery cost in Vizag ● low-cost fissure surgery in Hyderabad ● cashless fistula treatment near me ● painless piles surgery in Vijayawada ● fissure treatment with insurance in Vizag ● fistula removal surgery cost in Hyderabad ● affordable piles treatment near me ● fissure laser treatment clinic in Hyderabad ● best fistula surgery cost in Vijayawada ● piles treatment hospital near me ● fissure laser operation price in Hyderabad ● low-cost piles laser treatment in Vizag ● fistula removal cost near me ● piles treatment with EMI in Vijayawada ● fissure surgery specialist near me
Disclaimer: **The result and experience may vary from patient to patient.. ***By submitting the form or calling, you agree to receive important updates and marketing communications.
Getting an accurate diagnosis can be one of the most impactful experiences that you can have.

cure with care
Copyright © 2025. All rights reserved.
Consult with our expert surgeon for more than 50+ diseases
Happy Patients
Hospitals
Cities