These are a common yet often overlooked condition caused by swollen rectal tissues and veins. At Heptacare Health, we offer advanced, painless treatment with cutting-edge technology. Get expert care and lasting relief book your consultation today.
Happy Patients
Disease
Hospitals
Cities
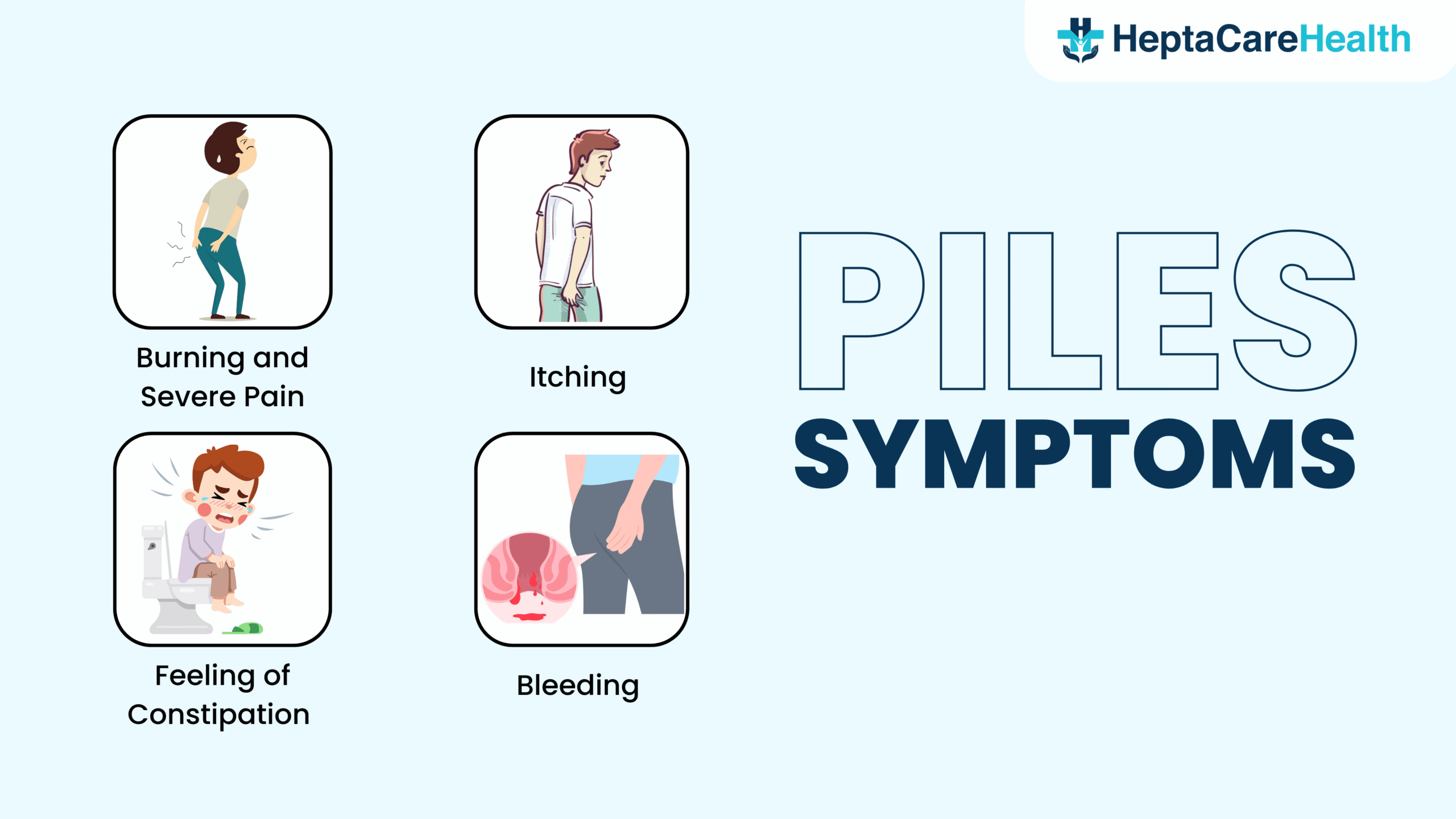
Piles, or haemorrhoids, develop when veins around the anus and lower rectum become swollen. They occur either internally (inside the rectum) or externally (around the opening of the anus). People of all age groups and genders can develop piles. However, medical records show that individuals between the ages of 50 and 60 are more likely to experience this condition.
Piles usually do not pose a serious medical concern and often improve with lifestyle changes and home remedies. You can ease symptoms by eating a high-fibre diet, drinking plenty of fluids, practicing good hygiene, applying over-the-counter creams or ointments, and avoiding straining during bowel movements. In rare and severe cases, doctors may recommend surgical intervention.
Heptacare Health means it’s management and treatment through expert consultation and advanced treatment modalities.At Heptacare Health, our team specializes in minimally invasive and laser-assisted procedures to minimize pain and promote faster recovery. We leverage the latest advancements in treatment and deliver a personalized approach focused on our patients. Whether your symptoms are mild or severe, our experts will help return your comfort and confidence. Schedule a Consultation You Deserve in Chicago, IL.
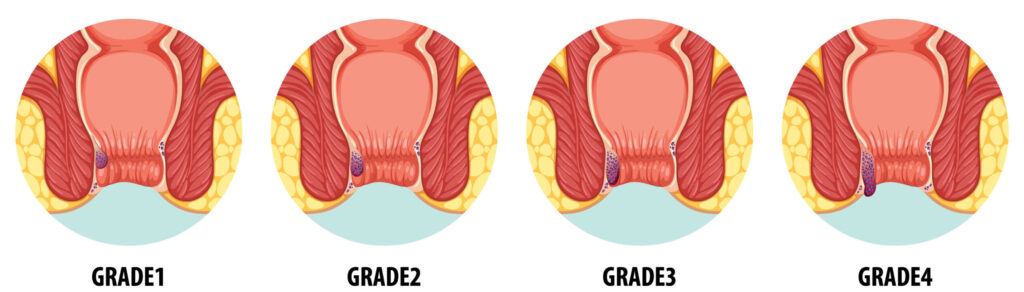
Internal piles develop inside the rectum, above the dentate line. They do not appear externally and are classified into different grades based on their severity and prolapse.
Grade 1:
Grade 1 represents the mildest form of internal piles. These small swellings stay within the rectal lining and do not protrude from the anus. Most people with Grade 1 piles experience no symptoms. Doctors usually recommend conservative treatments like lifestyle changes, sitz baths, and topical ointments or creams.
Grade 2:
Grade 2 piles are larger than Grade 1 and may protrude during bowel movements. However, they retract back into the rectum on their own after defecation. Doctors often treat Grade 2 piles using non-surgical methods such as rubber band ligation, infrared coagulation, or sclerotherapy.
Grade 3:
Grade 3 piles also prolapse during bowel movements but don’t retract automatically. Patients must manually push them back into the rectum. These piles often cause discomfort, pain, itching, bleeding, and hygiene challenges. Treatment options typically include rubber band ligation, infrared coagulation, or sclerotherapy.
Grade 4:
Grade 4 piles represent the most severe and advanced stage. They remain outside the anus and cannot be manually repositioned. These piles appear large, inflamed, and highly sensitive. Many patients suffer from severe pain, continuous bleeding, and hygiene difficulties. Complications such as thrombosis (blood clots) or strangulation may also occur. In most cases, surgeons recommend procedures like laser surgery or stapled hemorrhoidectomy to treat Grade 4 piles effectively.
A proctologist or an anorectal surgeon can diagnose piles by taking your medical history, performing a physical examination, and conducting diagnostic tests if necessary. Here’s an overview of the diagnostic process:
Medical History:
Your healthcare provider will begin by asking about your symptoms, including any pain, itching, bleeding, or changes in bowel movements. They will also review your medical history and inquire about any previous episodes of piles.
Physical Examination:
The healthcare provider will examine the anal region to check for external and internal piles. They may visually inspect the area and gently insert a gloved finger into the anus and rectum to feel for abnormalities, swelling, or lumps.
Digital Rectal Examination (DRE):
In certain cases, the provider may perform a digital rectal examination. During this procedure, they insert a lubricated, gloved finger into the rectum to evaluate internal piles and identify any other rectal issues. The examination usually takes only a few moments and causes minimal discomfort.
It’s can be treated using both non-surgical and surgical methods. Here are some common non-surgical and surgical treatments:
Non-surgical treatments:
Rubber band ligation:
Rubber band ligation is a commonly used non-surgical treatment for internal piles. To perform this procedure, a doctor inserts a viewing scope (anoscope) into the anus. Then, a special instrument called a ligator is used to place a small rubber band at the base of the piles. As a result, the blood supply to the piles is cut off, causing them to shrink and eventually fall off within a few days. Typically, the procedure takes about 30 minutes, and patients can go home afterward. Moreover, the recovery time is short, and most individuals can resume their normal activities within a few days.
Sclerotherapy:
Among the wide range of treatment options for managing piles, a non-surgical modality is sclerotherapy. In this technique, a solution (sclerosant) is injected into the affected vein, causing it to shrink and eventually fade away. It is important to note that sclerotherapy is typically used for internal piles. Furthermore, since it is a non-surgical procedure, it generally offers a faster recovery time compared to surgical interventions.
Infrared photocoagulation:
Infrared photocoagulation is a medical procedure for treating small and medium-sized piles. Notably, this treatment is only suitable for internal piles. During the procedure, the doctor uses a device that produces an intense beam of infrared light. The heat generated causes scar tissue, which cuts off the blood supply to the piles. Consequently, the piles shrink and eventually fall off. Scar tissue then forms on the wall of the anal canal. This scar tissue helps hold nearby veins in place so they don’t bulge into the anal canal. Additionally, the recovery time is typically short, and most individuals can resume their normal activities immediately after the procedure.
Electrocoagulation:
This procedure uses an electric current to destroy the piles. To begin, a proctoscope is placed in the anus to locate the piles. A probe is then positioned at the base, and an electric current is delivered using a handpiece connected to the probe. The aim is to thicken the blood in vessels and cauterize it at the base. As a result, the piles start to shrink. However, recovery time can vary from person to person, depending on factors such as the size and severity of the piles, as well as individual healing capabilities.
Anoscopy or Proctoscopy: These procedures involve using a small, lighted tube called an anoscope or proctoscope to examine the anal canal and rectum more closely. Anoscopy and proctoscopy directly visualize the anal canal and rectum, allowing for a more detailed examination of piles and other rectal disorders. These procedures can help determine the location, size, and severity of the piles, guiding the healthcare provider in developing an appropriate treatment plan.
Sigmoidoscopy: In this procedure, the healthcare provider uses a sigmoidoscope (lighted tube with a camera) to view the lower part of the colon and rectum. Procedure types include flexible sigmoidoscopy and rigid sigmoidoscopy. Flexible and rigid sigmoidoscopy allows healthcare providers to directly visualize the rectum and lower sigmoid colon, aiding in identifying various conditions, including piles.
Colonoscopy: Colonoscopy helps examine the colon or the large intestine to check the abnormalities inside it. A colonoscopy evaluates rectal bleeding due to piles or other causes and rules out more serious problems so the doctor can suggest the most appropriate treatment for piles.
Surgery is the best and most sure-shot method of piles treatment. Piles need surgery in cases where home remedies, medications, and other conservative measures have failed to provide relief or when the piles are severe or persistent. Some common types of piles surgery include:
Open surgery–Open surgery, or open hemorrhoidectomy, is a traditional surgical procedure to remove piles. In this procedure, the surgeon makes an incision in the anal region to locate the piles. The incision is generally made around the anus or in the anal canal, depending on the location and severity of the piles. The surgeon carefully removes the piles using surgical instruments, and the technique may involve excising the piles or ligating them with sutures to restrict their blood supply. The goal is to completely remove or reduce the size of the piles. The complete recovery time after open surgery for piles can vary from several weeks to a few months. It depends on factors such as the extent of the surgery, individual healing abilities, and adherence to post-operative care instructions.
Stapler surgery- Stapler surgery or stapled hemorrhoidectomy is a surgical method for treating piles. It utilizes a stapling device to remove piles tissues. Doctors suggest this treatment procedure for patients whose piles have prolapsed or become abnormally large or who have shown little or no improvement with nonsurgical treatment. Under stapler surgery, the piles tissue is lifted into a ring of tissues with sutures, and a stapler removes it, restricting blood flow to the tissue.
As a result, patients who undergo stapler surgery typically experience less pain than those who undergo traditional piles surgery. They also experience less bleeding, itching, and swelling around the anus and inside the rectum. Recovery from stapler surgery is quick and is linked to fewer complications.
Laser surgery– Laser surgery is the safest and most effective surgical option. This procedure uses laser energy to shrink and coagulate the piles tissue. However, the surrounding healthy tissues remain unaffected. Laser surgery is a minimally invasive approach performed on an outpatient basis. It is associated with minimal post-operative pain and a relatively shorter recovery time.
Laser surgery is a much safer, quicker, and more effective surgical option for removing piles compared to any other treatments.
Laser surgery, also known as laser hemorrhoidectomy or laser hemorrhoidoplasty, is a minimally invasive surgical procedure used to treat piles. One of the best advantages of this surgery is that it results in minimum bleeding, making it a good option for curing piles. Other advantages of laser piles surgery include the following:
Less painful and safe procedure- When we talk about any surgical procedure, the first thought that crosses our minds is the pain it inflicts on the body. Laser surgery is one of the least painful surgical methods to treat piles.
Quick procedure- Removal of piles using laser surgery is quicker than other surgical techniques of removing piles. Laser surgery takes around 30 minutes, depending on the location and number of piles to be removed. Also, the person will be allowed to go home soon after the surgery and will not require a hospital stay.
Reduced risk of infection- The use of laser energy can help sterilize the treated area, lowering the risk of infection.
Quick healing- Minimal blood loss and lower chances of infection during the surgery lead to quick healing of the treated area.
High success rates- Laser surgery has shown high success rates in treating piles. It can effectively remove or shrink piles tissues, providing long-term relief from symptoms like pain, itching, bleeding, and discomfort.
Minimal postoperative discomfort- Laser surgery is linked with minimal postoperative pain and discomfort compared to open surgery. This can result in a more relaxed recovery period for patients.
Lower risk of incontinence- Laser surgery targets the piles tissue precisely, reducing the risk of damage to the surrounding anal sphincter muscles. This can help reduce the risk of postoperative incontinence, a potential complication of other surgical procedures.
Lower risk of recurrence- Laser surgery effectively treats the underlying piles tissue, reducing the likelihood of recurrence in comparison to non-surgical or conservative treatment methods.
Prior to your treatment, your proctologist will likely instruct you to take some precautions and follow some guidelines. These typically include:
Like any surgical procedure, piles surgery can have potential side effects and risks. Here are some possible side effects associated with piles surgery:
Advantages
Minimally invasive – Laser surgery for piles is often minimally invasive, requiring smaller incisions compared to traditional surgery, which can result in less post-operative pain and faster recovery.
Reduced bleeding – The laser cauterizes blood vessels as it cuts, leading to reduced bleeding during and after the procedure.
Precise targeting – Laser surgery allows for precise targeting of hemorrhoidal tissue, minimizing damage to surrounding healthy tissue.
Shorter recovery time – Patients undergoing laser surgery for piles typically experience a shorter recovery time compared to traditional surgical methods.
Reduced risk of complications – The precision of laser surgery can reduce the risk of complications such as infection and tissue damage.
Disadvantages
Expensive – Laser surgery for piles can be more expensive than traditional surgical methods, as it often involves specialized equipment and expertise.
Limited availability – Not all healthcare facilities offer laser surgery for piles, limiting access for some patients.
Chances of recurrence – While laser surgery can effectively remove hemorrhoidal tissue, there is still a risk of recurrence of hemorrhoids over time.
Side effects – Some patients may experience side effects such as temporary pain, discomfort, or swelling after laser surgery for piles.
A proctologist or a general surgeon is considered to be the best doctor for piles surgery. A proctologist is a medical professional with a specialization in the diagnosis and treatment of colorectal disease and conditions. These include conditions relating to your colon, rectum, and anus.
Diagnosis
In the case of external piles, the doctor can diagnose them with a physical inspection. However, in case of internal hemorrhoids, the proctologist will perform a digital examination to insert a gloved, lubricated finger into the rectum to check for abnormal growth. Additionally, to correctly diagnose internal piles, the surgeon may choose a proctoscope, an anoscope, or a sigmoidoscope to examine the lower rectum.
Laser Surgical Treatment
Laser-assisted surgery for piles is one of the most efficient treatment methods. During the procedure, a focused narrow beam of light is used on the hemorrhoid to ablate or shrink it without affecting the surrounding tissues. It is an advanced, minimally invasive procedure that aids the patient’s faster recovery.
You must also keep in mind the following:
Some of the best ways to treat piles without surgery include:
Home Remedies
There are multiple home remedies to help you reduce the pain and swelling associated with piles. The results may not be permanent or quick, but they can help reduce the pain and other symptoms in the early stages of piles. Here are some of the most effective home remedies:
Several medications can help manage the symptoms of hemorrhoids effectively. Below are some commonly recommended options:
Oral Pain Relievers:
Over-the-counter painkillers, such as acetaminophen or ibuprofen, can help ease discomfort. However, it’s crucial to follow the recommended dosage. If you have underlying medical conditions or are on other medications, make sure to consult a healthcare professional before use.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
NSAIDs, including ibuprofen or naproxen, not only relieve pain but also reduce inflammation. Nonetheless, they should be used under medical supervision due to potential side effects.
Medications to Enhance Blood Circulation:
In some cases, doctors may prescribe venotonic or vasoprotective agents. These medications improve blood circulation and strengthen blood vessels in the rectal area. As a result, they can reduce symptoms and help prevent further complications.
Vasoconstrictors:
Medications containing vasoconstrictors, such as phenylephrine, are available in topical or suppository form. These work by shrinking blood vessels and reducing swelling. Therefore, they are often recommended for symptom relief.
Fibrinolytic Agents:
In certain situations, fibrinolytic agents are used to dissolve clots that form within external hemorrhoids. Typically, a healthcare professional administers these medications via injection. Consequently, they are not suitable for home use.
Antibiotics (Amoxicillin-Clavulanate):
When infection is present, medical treatment becomes essential. Amoxicillin-clavulanate is one of the most effective antibiotics for infected hemorrhoids. It helps by targeting bacteria responsible for the infection and supports the healing process.
Choosing the right foods can significantly ease symptoms and support recovery. Below are foods that are beneficial for managing hemorrhoids:
Flavonoid-Rich Foods:
Foods rich in flavonoids—such as citrus fruits (oranges, lemons), berries, cherries, and dark chocolate—may help strengthen blood vessels and decrease inflammation. As a result, these foods can provide relief from discomfort.
Healthy Fats:
Include sources of healthy fats in your meals, such as avocados, seeds, and olive oil. These fats help lubricate the stool, making bowel movements smoother and less painful.
Probiotic Foods:
Additionally, consuming probiotic-rich foods like yogurt, kefir, and sauerkraut can promote a healthy gut microbiome. In turn, this improves digestion and reduces the risk of constipation.
Adequate Fluid Intake:
Drinking plenty of fluids throughout the day keeps the body well-hydrated. Consequently, this helps soften stools and supports regular bowel movements.
Vegetables:
Eat a wide variety of vegetables, including leafy greens like spinach and kale, as well as broccoli, brussels sprouts, carrots, and cauliflower. Because these vegetables are high in fiber, they promote healthy digestion and reduce the risk of straining.
Whole Grains:
Moreover, incorporate whole grains such as oats, brown rice, quinoa, and whole wheat products into your daily meals. These are rich in fiber and help add bulk to your stool, which eases bowel movements.
Legumes:
For example, lentils, chickpeas, black beans, and kidney beans are excellent sources of fiber. Adding legumes to your diet helps prevent constipation by softening the stool and reducing strain—which is particularly important for relieving hemorrhoid symptoms.
Nuts and Seeds:
Lastly, nuts and seeds like almonds, walnuts, and chia seeds can support digestive health. Not only are they fiber-rich, but they also offer anti-inflammatory benefits, which may help reduce swelling in affected tissues.
Meat:
Red and processed meats lack fiber, digest slowly, and contain high amounts of sodium. These qualities often lead to constipation, which can worsen hemorrhoid symptoms.
Spicy Foods:
Spicy dishes, hot peppers, and sauces irritate the digestive system. They can intensify itching, burning, and inflammation. Limiting spicy food helps reduce discomfort.
Alcohol:
Alcohol dehydrates the body and contributes to constipation. Reducing or eliminating alcohol supports smoother digestion and recovery.
Processed Foods:
Fast food, packaged snacks, and processed meats usually contain little fiber and many unhealthy fats and additives. These foods can slow digestion and increase the risk of constipation.
Low-Fiber Foods:
White rice, white bread, plain pasta, and noodles produce smaller, harder stools. This increases straining during bowel movements, which puts pressure on abdominal veins and can aggravate hemorrhoids. Replace these with fiber-rich choices like whole grains, fruits, and vegetables.
Sugary Foods:
Candies, pastries, and sugary drinks contribute to constipation and upset the gut’s bacterial balance. Instead, choose fruits that offer natural sweetness, hydration, and fiber.
After surgery, the anal area becomes very sensitive. Rest and follow your doctor’s instructions closely to support a smooth recovery.
Keep the Area Clean:
After each bowel movement, rinse with warm water or take a sitz bath. This soothes the area, improves blood flow, and eases discomfort. Use gentle wet wipes and avoid harsh rubbing.
Manage Physical Activity:
Avoid heavy lifting or strenuous activity for 2–3 weeks. Light walking helps circulation without adding pressure to the surgical site.
Take Medications as Directed:
Follow your doctor’s guidance for pain relievers, antibiotics (if necessary), and stool softeners or laxatives to prevent straining.
Use Cold Compresses:
Apply a cold pack wrapped in cloth to the area for short periods to reduce swelling and relieve pain.
Sit Properly:
Use a cushion or donut-shaped pillow to reduce pressure when sitting.
Eat Mindfully:
Avoid greasy, spicy, or junk food during recovery. These foods can cause constipation or diarrhea, which may interfere with healing.
Some possible complications of piles include:


Based on 7721 Recommendations | Rated 4.68 Out of 5
Happy Patients
Clinics
Cities
Surgeries
Doctors
Hospitals

Get relief from painful proctology with advanced laser treatment.
Minimally invasive, no stitches, same-day discharge…
Heal painful anal fissures with advanced, non-surgical care.
Quick relief, minimal downtime, expert proctology support…
Treat anal fistula with safe, advanced procedures.
Minimally invasive care with faster recovery.

Get permanent relief from pilonidal sinus with laser surgery.
Painless procedure, quick healing, same-day discharge.

Advanced treatment for rectal prolapse by expert surgeons.
Safe procedure, minimal pain, long-term relief.

Common symptoms include itching, pain during bowel movements, bleeding, and swelling around the anus.
Yes, most health insurance plans cover piles surgery, including laser treatment.
Eat a high-fiber diet, drink water, avoid straining during bowel movements, and exercise regularly.
It’s a safe and effective method with minimal side effects and faster healing than traditional surgery.
● piles laser surgery cost in Vizag ● low-cost piles surgery in Hyderabad ● cashless piles treatment near me ● painless piles surgery in Vijayawada ● piles treatment with insurance in Vizag ● piles removal surgery cost in Hyderabad ● piles operation packages in Vijayawada ● affordable piles treatment near me ● piles laser treatment clinic in Hyderabad ● piles doctor consultation charges in Vizag ● best piles surgery cost in Vijayawada ● piles treatment hospital near me ● piles laser operation price in Hyderabad ● low-cost piles laser treatment in Vizag ● piles removal cost near me ● piles treatment with EMI in Vijayawada ● piles surgery specialist near me ● piles surgery packages in Hyderabad ● piles treatment clinic near me ● piles laser surgery near me
Disclaimer: **The result and experience may vary from patient to patient.. ***By submitting the form or calling, you agree to receive important updates and marketing communications.
Getting an accurate diagnosis can be one of the most impactful experiences that you can have.

cure with care
Copyright © 2025. All rights reserved.
Consult with our expert surgeon for more than 50+ diseases
Happy Patients
Hospitals
Cities